Two severe H5N1 cases caused by the D1.1 genotype are reason for increased concern.
That and other stories in "Five on Friday" for December 20, 2024...
Item 1: H5N1 updates. Two active cases that bother me more than the rest.
There have been 61 cases of avian influenza (H5N1) in the United States during the massive outbreak that has swept its way through herds of dairy cattle, birds, and other animals. Remarkably, until yesterday all of them had been mild. There have likely been many more cases, but it’s almost certain that they were also mild, if not asymptomatic.
Yesterday, the CDC announced that the first severe case of H5N1 has occurred in a Louisiana man, who is older than age 65 and has some medical problems. However, he was in his backyard when he was exposed to an infected bird, which gives some indication that he was previously healthy enough to be out and around.
This case concerns me because we’ve been told that it was caused by the D1.1 genotype of H5N1. That’s the same version as the one that infected an apparently otherwise healthy teen in Canada who became so sick that he required intubation and mechanical ventilation for a prolonged period. Together, these two D1.1 cases have raised my interest in this story (albeit there have been a few mild cases of this genotype as well, occurring in Washington State.)
While this strain is not the one causing the numerous large outbreaks among US animals, the case shows that there are other ways to get H5N1 and that severe disease is possible.
I spent a large part of my week on a deep dive to understand where things stand from scientific and policy perspectives. I spoke to officials in the White House, the CDC, and other experts I trust. I’ll have more to say on this in the coming days, but suffice it to say that my level of concern is markedly higher than it was previously, although we are not yet at “DEFCON 1.”
The one good piece of news is that so far, there has been no human-to-human transmission of H5N1. If that starts happening, we could be in trouble.
Reminder: Please get your flu shot. While it likely won’t prevent bird flu, it will prevent a coinfection of bird and seasonal flu—which could be very bad indeed.
Here’s my segment on CNN yesterday in which I discussed the situation.
Item 2: Trump world debate on GLP-1s vs. lifestyle ignores the science.
An article in the New York Times describes a big debate in the Trump world about whether GLP-1 medications like Ozempic, Wegovy, Mounjaro, and Zepbound are better than lifestyle modifications in the treatment of obesity.
I found this to be rather bizarre. This is settled science. In some of the most important blockbuster studies demonstrating the impressive efficacy of the GLP-1 class of medicines, the various drugs and doses were tested against placebo recipients who also received intensive lifestyle modification counseling. That was true in major studies of obesity. The same was true in a study of heart failure and diabetes control. The same was true in a major study of knee pain in people with arthritis. The list goes on and on.
In all of these studies, people injecting placebo lost a little bit of weight at first. Part of that was the placebo effect and part of that was the reality of receiving excellent lifestyle (diet and exercise) counseling provided to all study participants.
The conclusion is obvious. For patients who meet the criteria of these studies (which is a substantial portion of the US population, by the way), the debate is over. The GLP-1’s are superior to lifestyle and diet changes alone. We’ve been trying lifestyle modifications for decades. Doctors can’t stop talking about these things! Diet and exercise help but it’s clear that they are not enough given today’s addictive and low cost food supply. It’s time to stop hemming and hawing about all of this and instead focus on how to make these drugs more affordable for those that need them.
Item 3: Ebola vaccine data shows effectiveness.
A study in the New England Journal of Medicine reports that the Ebola vaccine (VSV-ZEBOV-GP, or “ZEBOV”) appeared to be effective in curbing mortality in recipients. While the study was not randomized (because it was felt that it would be unethical to deny the placebo group a vaccine that was already believed to be effective), the study design allows some fascinating inferences.
Researchers followed vaccine recipients over time. In the first 9 days after receiving ZEBOV, the case fatality rate (that is, the number of deaths divided by the number of cases) among those who became infected was 26% (99 deaths out of 385 cases)—a staggering figure, although on the low end for Ebola outbreaks (likely because many of the participants were healthier than the general population). From there, things got better. From days 10-29, the case fatality rate was nearly cut in half, dropping to 14% (5 deaths out of 35 cases). For those who were infected 30 days or longer after ZEBOV vaccination, the case fatality rate was 5% (2 deaths out of 42 cases). This strongly suggests that as the immune system responded to the vaccine, the effectiveness increased.
It’s especially impressive to me that both the case fatality rate and the number of cases fell, the longer after vaccination the researchers looked. Often, during outbreaks, case counts increase dramatically a few weeks into the emergency because awareness of that outbreak leads to more testing. That tends to lead to lower (and, frankly, more accurate) case fatality rate data later in the outbreak. But here, the case counts actually went down, despite close follow up (if the case counts went down because the researchers lost track of the recipients, that would sully these results. That is not what happened here). This means the lower case fatality rate later in the study (i.e., longer after vaccination) was not an artifact of increased testing.
This is great news for future Ebola outbreaks. Still, a disease with a 5% case fatality rate is extremely scary.
Item 4: Brrrr! Climate change deaths due to extreme cold.
New research in the Journal of the American Medical Association shows that deaths due to extremely cold temperatures have increased this century in the US. The rates are highest in the Midwest, which is the coldest region in the country, though rates have increased everywhere else too (Northeast, South, and West).
Climate change is not just “global warming.” It’s also extreme weather (as my colleagues and I have pointed out related to wildfires). So, it’s not a surprise to see these data. While the rates are “low”—at less than 1 per 100,000 people per year—things have taken a significant turn for the worse since 2018. The study authors are not sure why the sudden change occurred but economic factors including homelessness and substance use were mentioned.
Item 5: Poll of the Week results.
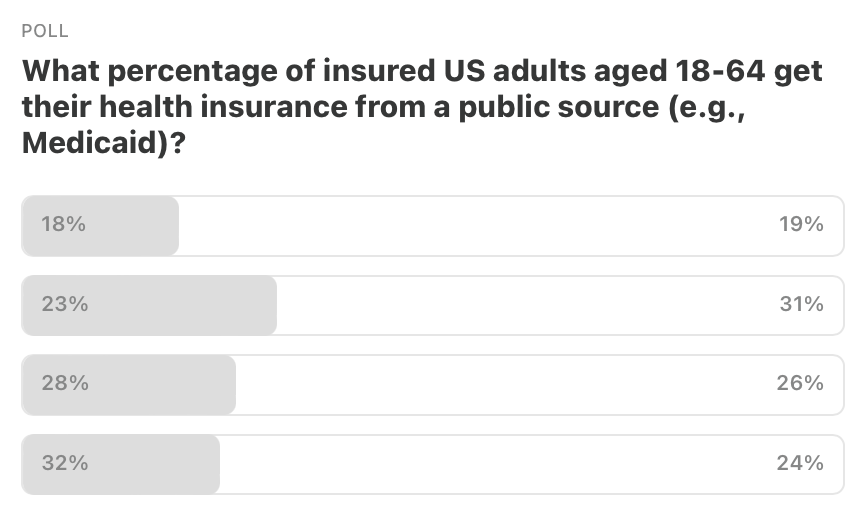
Here are the results to last week’s poll. The correct answer was 23%, which a plurality of you got right. Nice work!
Item 5a: Poll of the Week!
The first human case of H5N1 was discovered in Hong Kong in 1997. But the first case among animals was described way back in 1878.
That’s it. Your “Friday Five!” Questions? Comments? Please chime in!
Feedback! Have any ideas for next week’s Poll of the Week? Any great articles you’ve read elsewhere that you want to share with the Inside Medicine community?







In your CNN segment, I was surprised that you didn't address the danger of drinking raw milk more directly - it seemed that the host set that one up for you, but you talked more generally about avoiding things that might be problematic. Given Kennedy's advocacy for raw milk, I'd like to see lots of direct contradiction of his position with specifics, which you certainly can supply.
What’s the latest with the H5N1 vaccine development (my kids age 15-26) are asking? I think 🤔 we read that Finland has this vaccine (is this true)? Wondering how other countries are preparing etc.. Thanks