Officially, influenza season begins in Week 40 of the calendar year, which corresponds to the first week of October. But most years, cases remain very low until December (or November in some years), when they start to rise rapidly. In my view, “real” flu season begins in earnest at some point when a “critical mass” of cases are circulating. When enough people have the flu, something changes, epidemiologically: Many chains of transmission begin simultaneously working their way through communities, and overall rates start to increase dramatically.
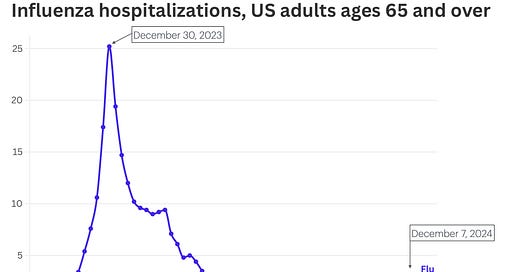
In many places in the US, we are just starting to see a takeoff in flu hospitalizations, which in turn tells us what’s happening in the surrounding communities. Here’s the latest for US adults ages 65 and up. Notice the increase in the last couple of weeks. This is classic for this time of year. It also matches what I’m seeing clinically in the ER, with a few cases starting to show up during my shifts over the last couple of weeks
If you want to check things in your area, the Inside Medicine Covid-19 and Respiratory Virus Metrics Dashboard is up-to-date: check it out here. Things are rather different in various places.
TL;DR: Now’s the time to start taking flu season seriously. Winter is coming.
Flu season looks to have arrived. But it’s still early…
For each demographic, what constitutes a critical mass of cases sufficient to drive a rapid increase in the coming days and weeks is different, and frankly, subjective. In this piece, I’m proposing that for people age 65 and older, a useful “point of no return” threshold might be 2 hospitalizations per 100,000 people.
Take a look at data from this season and the four preceding ones (excluding 2020-2021 and 2021-2022, when we essentially obliterated flu due to Covid-19 mitigation; turns out infection control measures work, when we try).
The red bars show the time between the first week in which at least 2 hospitalizations per 100,000 people ages 65+ occurred and the eventual peak of that season. That time span ranged from 6 to 13 weeks, depending on the year. You can see that we just crossed the threshold in the most recent week of data, with 2.9 per 100,000 seniors hospitalized with flu during that 7-day period (see the “We Are Here” arrow on the bottom right panel).

There are two reasons I chose 2 hospitalizations per 100,000 seniors as the “line in the sand”/time to raise awareness flag on flu season. First, once this level is reached, it’s virtually guaranteed that cases will soon climb dramatically to an eventual peak (the above graphs show that). Second, the timing is right: not too soon to be alarmist but in time for people to do something useful with the information. While two flu-related hospitalizations per 100,000 people isn’t nothing, it’s a tiny fraction of the eventual peak in this age group. Usually, the worst week of the year surpasses 1,000% of the 2 hospitalizations per 100,000 threshold in this demographic.
So…
It’s time to act.
If the public were to be alerted to this milestone—like we are doing here on Inside Medicine—it might have a public health benefit. Indeed, there are helpful things we can do with this information.
1. Vaccination reminder. Now’s better than ever.
First, anyone who has not yet been vaccinated against flu this season, this is your nudge to go do it now. Let me say that a little louder…
If you haven’t received your annual influenza vaccination, *now* is the time!
In fact, as I wrote in the New York Times earlier this fall, those procrastinating until now have actually timed things perfectly, provided they actually go and get it now. Influenza vaccine effectiveness peaks within a couple of weeks of receipt and wanes steadily after that. Anyone getting their shot today will likely have peak protection during late December and early January, right when we often see massive peaks. And even if the peak is in February or early March, the waning won’t be as dramatic as for those of us who received shots earlier. (I’m required to get mine by late October, sadly; I’d rather have waited until now.)
2. Behavioral choices/changes can be data-driven.
In addition, rising influenza levels may trigger people to change their behaviors. For example, some people are done with masking most of the time, but are willing and even interested in throwing one back on in crowded situations during massive waves of flu (or Covid, or RSV). Some people might even choose to skip extremely crowded indoor events during local waves. But, there’s nuance here and it’s highly situational. For example, I simply could not forgive myself if I missed my fall chorus concert due to one of these illnesses. If I knew flu (or Covid) cases were high, I might personally choose to skip out on a crowded event I was on the fence about attending anyway. Deciding what events to skip depends on your own risk tolerance, how important the event is to you, the configuration (i.e., will there be lots of loud people in a small space? Or just quiet ones in a huge space?), and whether masking is feasible.
3. Choosing when to use pricey at-home tests.
We have all become comfortable with the concept of rapid at-home Covid tests. There are now rapid flu and RSV tests too. With rapid flu tests becoming a bit more common (albeit still prohibitively expensive for many people), knowing when we are really headed into flu season might help people decide when to use the tests they decide to buy. Let’s say you visit an immunocompromised relative once per week. If you bought 6 rapid flu tests for $53, you might not want to waste them when local levels are low. But knowing we’ve entered a period when we expect flu to skyrocket might drive a choice to use them.
Knowledge is power, and we’ve got you covered.
Take a look at our Inside Medicine Covid-19 and Respiratory Virus Metrics Dashboard. We update it every single week. You’ll find metrics on hospital capacity, Covid hospitalizations and wastewater for every US state, and flu, RSV and Covid data for select states in the CDC’s tracking system. And we’ll be adding some new functionality soon, if there’s continued interest. Stay safe out there, folks…
Thanks to Benjy Renton for keeping the Inside Medicine dashboard up and running…and better than ever.
Hi readers! Do metrics like these help inform your choices? Join the discussion and tell us your approach in the Comments section.




Love the dashboard!
Wear an N95 mask everywhere, NOW!