Good news for a "pain in the eyes" condition.
Scratched corneas hurt. Now we can make some of them less miserable.
Scratched corneas are so common that nobody has any idea what percent of the population has experienced one.
So, let’s start with a poll.
Now let’s get into corneal abrasions…
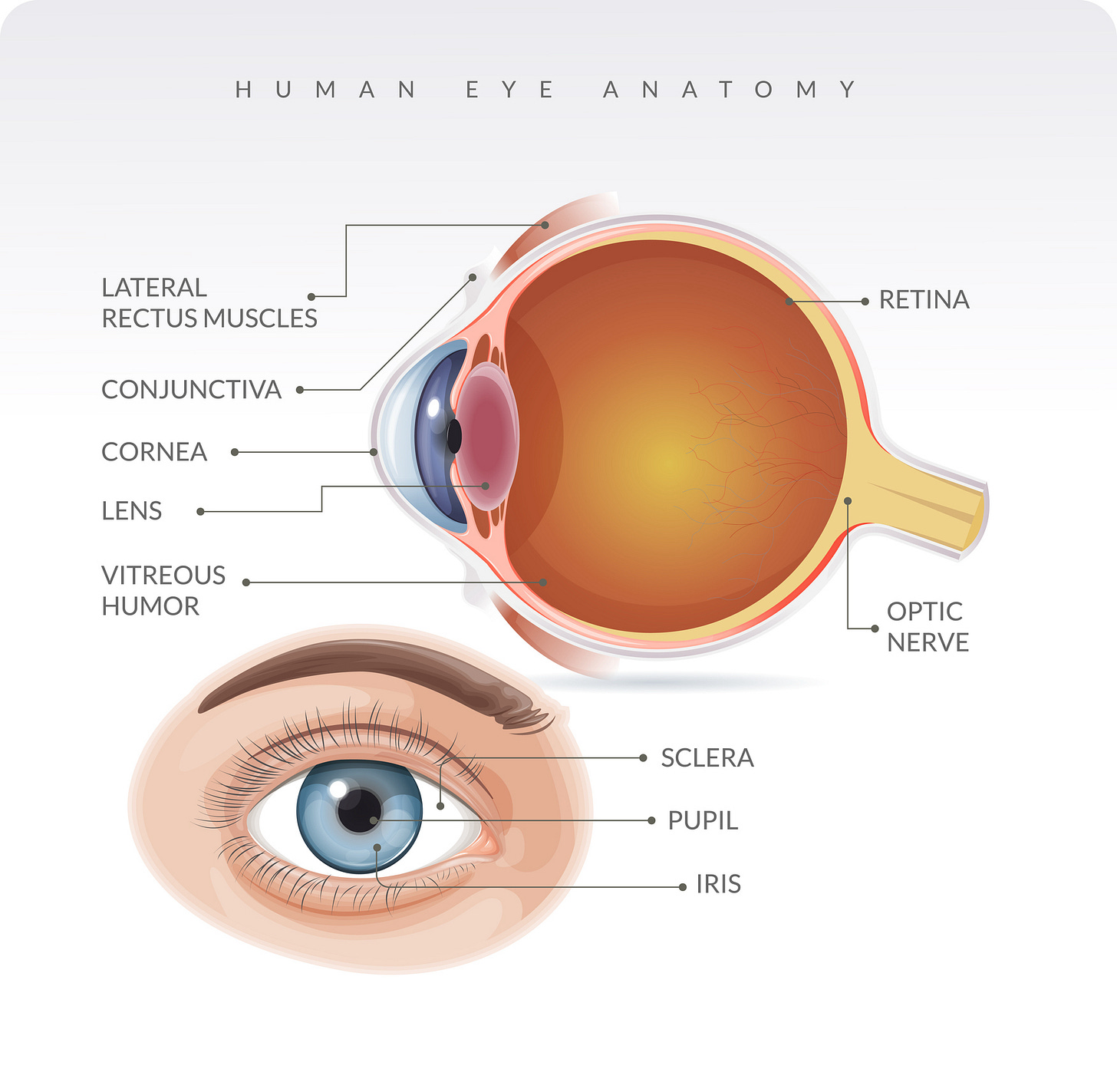
Anatomy: The cornea is the clear protective covering over the iris (i.e., the colored part) and the pupil (i.e., where light enters).
The injury: Scratched corneas, or corneal abrasions, are little cuts. Your cornea can get scratched by anything, from your fingernails to sawdust to microscopic metal shreds (welders, beware, because this can cause major problems). Even car airbags can cause corneal abrasions—although I emphasize that if an airbag hits your face, any damage caused is highly likely to be preferable to what would have happened if there had been no airbag. Scratched corneas hurt. They cause some tearing. Some redness may occur in the white of your eyes, but not always. Infections can occur, because the cornea’s main job is to be a protective barrier.
What you should do: First, if you think something is in your eye, rinse it out under running water from a faucet. If you still feel something, don’t go overboard hunting in there. The sensation of a foreign object in the eye (and elsewhere inside the body, while we’re at it), is often impossible for our brains to distinguish from small cuts.
If you suspect you have scratched your cornea, you should see a doctor as soon as you can. ERs and urgent care facilities are fine if you can’t get into an eye specialist. The reason you want to be seen is that sometimes things are more complicated than you might realize, and you want to be sure you don’t have a more serious injury or even an existing eye problem that a small injury happens to have unmasked. And if there’s any potential for a “foreign body” lodged in there, no matter how small, you need to have that diagnosed and addressed.
What we clinicians do: Generally, we doctors will numb your eye enabling us to put some dye in there for our examination. Then, under blue light (often using a special lamp, like in the photograph up top), we can see how bad the injury is. If it’s a simple abrasion, we might prescribe some antibiotics and anti-inflammatory pain relief medication. Eye patches are no longer recommended. If you wear contact lenses, the doctor may prescribe something different, so make sure to alert your clinicians if you wear them.
What most doctors do not do (but maybe can!): The dogma we clinicians were taught is very strong here. “Thou shalt not give or prescribe patients any more numbing eye drops to go home with, lest this delay wound healing and lest this mask their pain instead of letting them realize over the next few days that they have an unusual and potentially bad complication, such as an ulcer or worsening infection.”
What some doctors like me do. Early in my career, I noticed the immediate relief patients got from the numbing drops. Like…a lot. They would ask if they could have that bottle of drops to take home. I’d say no. But over time, I heard that it was probably safe to give patients some of the medication “to go.” To address the concern that a patient I gave the drops to might up being harmed by that, I had a simple workaround: I emptied most of the medication into the sink. I handed the patients a bottle with just enough liquid for a few more doses. If they used it all in the next 24 hours, no big deal because they’d come back the next day if something worse was emerging. If they spread the doses out over a longer period, no big deal because they’d be in too much pain between doses to tolerate life at home anyway. In other words, I gave them enough medicine to help them through the worst of it, but not too much to risk them ignoring any important complications that would require a second visit. My patients love me for this, and the limited supply I provide keeps it safe.
Apparently, however, this makes eye doctors break out into sweats. However, the rare cases (in the medical literature) where things have gone wrong have clearly been ones where overuse of the numbing drops over many days led to (or masked) big problems. My workflow explicitly avoids that.
Data support doing it my way! Turns out that there are some studies that support my way of doing things. I’m hardly the only doctor who has been doing this, albeit I still find that most do not. Good news! A new guideline from the American College of Emergency Physicians says that my approach is safe.
Caveats. For the pain of corneal abrasions to be safely treated with a short course of numbing drops, there are some essential features:
The abrasion must be “simple" and not too large. (You’ll need this to be diagnosed by a doctor, whether in an ER or elsewhere). There can be absolutely no other injury, nor any sign of damage to deeper structures.
No chemical or thermal causes. No UV light-caused injury.
No gross contamination, infections, or retained foreign bodies (including any “rust ring” after an object has been removed.
No underlying corneal diseases or existing damage.
No history of herpes of the eye.
No previous corneal surgeries or transplants to that eye, and no other ocular surgery within the last month.
The data on the safety of sending people home with these drops do not apply to kids. (We just do not know, either way.)
Nuance and concluding thoughts: There remains some controversy in the field about this. I’ll leave that for another day. But if you ask for numbing drops “to go” and your clinician refuses, it’s possible that they either are not up to speed on the latest guidelines or they have another concern that is giving them pause. So, if they refuse to prescribe numbing drops, don’t be too upset at them. But suffice to say that if I ever scratch my cornea (again; oof, the first time was not fun), I’ll get enough numbing drops to tide me over for 24 hours. I’ll also follow up with an eye doctor within 48-72 hours (as everyone should after scratching their cornea) for a repeat evaluation.
The most important thing is to realize when something isn’t going “as expected.” As long as a few doses of numbing drops does not prevent you from identifying any important complications, you’ll be in the clear.
Questions? Concerns? Angry statements from eye doctors? Leave them in the Comments!





I had a corneal abrasion in grad school. Ironically, I cut myself with the edge of my dissertation. It was one of the worst experiences. The ophthalmologist I went to did the FITC drop test on me and showed me the cut in the mirror. I have to say it was really cool to see the tiny glowing sliver in my eye. He prescribed me some antibiotic drops, and that was it. I went home, and basically had to sit in bed with my eyes closed the entire day, because my other eye was sympathetic, and stopped wanting to open. And it still hurt! The next day, I went to an optometrist. He took a look at my eye and prescribed a contact lens. That did the trick because the pain I was feeling was from my eyelid, rubbing against and continually opening the cut. My eye stopped hurting, almost immediately, and healed within 24 hours.
I would love to hear what Dr. Glaucomflecken would have to say about this!