Your at-home rapid test questions answered. Are five days of isolation with Omicron really enough?
Recent CDC guidelines have understandably confused a lot of people. Let’s clear it up before your free coronavirus tests arrive in the mail.

Last month, the US Centers for Disease Control and Prevention released new guidelines for the general public saying that those testing positive for SARS-CoV-2 could end their isolation after 5 days–regardless of vaccination status–provided they were asymptomatic or had symptoms that were improving.
A new genre on social media quickly emerged: people posting photographs of the results of their positive at-home rapid antigen tests, well after day 5 since diagnosis. Some were still symptomatic, many were not. Colleagues, random friends, strangers, and even CNBC’s Jim Cramer were in my DMs asking what to do with their positive results.
Could they end their isolation after 5 days, even if their rapid tests remained positive? No, I told them. But I couldn’t blame them for asking. The CDC’s guideline seemed to imply that. Specifically, the CDC said that infected people could end their isolation after 5 days (if asymptomatic or if symptoms had resolved) without further testing. But that’s not the same thing as saying nobody is contagious after 5 days. That’s not the same thing as saying to ignore a positive rapid test taken 5 days after diagnosis. But the confusion was understandable.
From the perspective of making sure society doesn’t grind to a screeching halt during a Covid-19 surge, the CDC’s guideline actually makes some sense. Better to have a few mildly contagious people out there wearing masks and keep grocery stores open, the reasoning seems to go, rather than insisting on longer isolation periods and having everyone clamoring for food if too many people get infected at once. But through the lens of personal safety, the new guidelines have proven themselves to be pretty inscrutable, even to educated people.
•••
With free rapid antigen tests now being delivered to US mailboxes (finally!), let me clarify the answers to the most frequently asked questions and tell you what you need to know about your rapid antigen test results.
Positive at-home rapid antigen tests. Key concepts: A positive at-home rapid antigen test at any time means you must consider yourself contagious.
•It doesn’t matter when you were exposed to or diagnosed with SARS-CoV-2. If the rapid is positive, you’re contagious.
•It doesn’t matter whether you are boosted, vaccinated, unvaccinated, or any of these in combination with a prior infection. (Note: this may change, but for now, there are too many unknowns). If the rapid is positive, you’re contagious.
•It doesn’t matter whether you have symptoms, whether your symptoms are getting better, getting worse, or even whether you ever had symptoms at all. To repeat: a positive rapid should not be ignored due to the absence of symptoms. If the rapid is positive, you’re contagious.
•It doesn’t matter whether the test result line is faint or strong. If the rapid is positive, you’re contagious.
•Rapid antigen tests still work for Omicron. Contrary to rumors, new data confirm that you don’t need to swab your throat. Nasal swabs, correctly done, remain adequate.
•False positives are possible. The best way to check for this is via a follow-up PCR test administered by a healthcare professional.

Testing before attending indoor events is effective!
•••
Negative at-home rapid antigen tests. Key concepts: A negative at-home rapid antigen test means you are unlikely to be contagious at the precise moment you took the test. (You’ll note the inverse of the “if the rapid is positive, you’re contagious” refrain above won’t appear below, because it does not apply to negative tests quite so neatly, sorry to say!)
•It doesn’t matter when you were exposed to or diagnosed with SARS-CoV-2.
•It doesn’t matter whether you have symptoms now, whether your symptoms are getting better, getting worse, or whether you ever had symptoms at all.
•False negatives are possible, but most negative rapids results are correctly negative; that is, the person might be infected but not contagious. If a rapid test is negative early or late in an infection (i.e. when the individual is not likely to be contagious), the result is not a false negative. It’s a true negative for contagiousness.
•However, the “warranty” on the reassurance provided by a negative rapid antigen test result (i.e. how long you can safely rely on that information) is highly variable, and does depend on the timing of your infection, as I’ll discuss below.
•••

A negative rapid antigen test (left) and a positive one (right).
Interpreting positive at-home rapid antigen tests.
It’s easy. If it’s positive, you’re contagious. Act accordingly to protect those around you.
Frequently asked questions about positive tests:
•Q: Does it matter how strong or faint the line is or how quickly the result becomes positive? A: Probably but we don’t know the specifics. A dark line appearing in a couple of minutes implies a more contagious source. However, I wouldn’t rely on that because how much virus the swab happened to pick up can be variable. If your test was more of a tickle, and less a lobotomy, a faint line might take more than 10 minutes to appear. But if that same tester had really gone for it (and folks, the swab should advance horizontally, not vertically), the same source might yield a darker line in just a couple of minutes. (This is another reason why the CDC’s guideline makes some sense from a public health standpoint. Most people who are contagious after 5 days are unlikely to be super-spreader-level contagious).
•Q: Why is my rapid test positive if I have no symptoms? A: Symptoms are mostly a reflection of your immune system fighting an infection, not the virus itself. Whether or not your immune system is suppressing the virus is simply not related to symptoms. Rapid tests are indifferent to this. They simply answer whether your body is emitting contagious virus. Any downplaying of a positive result because of mild or no symptoms is unwise. Also, those who think rapid tests can’t be used on asymptomatic people are incorrect.
•Q: If my rapid test is positive on day 6-10, when should I retest? When can my isolation period end? Realistically, how often you retest depends on how many tests you have. If you only have a couple left, I’d wait at least two days after a positive result before checking again. If your test line turns dark quickly, I might even wait 3 days. Ideally, you should have two consecutive negative rapid tests (again, no sooner than 5 days after diagnosis), and those negative tests should be at least a day apart before ending isolation. If symptoms are worsening, I wouldn’t retest until they’ve improved, unless you have plenty of tests that nobody else is going to use (which seems unlikely).
•Q: I heard that after 5 or 10 days, I might have a positive result on a rapid antigen test but no longer really be contagious. Is that true? A: No. Many people have confused a fact about PCR tests with one about rapid antigen tests. PCR tests diagnose infections (but do not indicate contagiousness, unless special further testing is done) by testing for RNA, the genetic material of the virus. Because the viral RNA can hang around for weeks, repeatedly testing positive on a PCR does not tell you if you’re contagious. The same is not true of rapid antigen testing; positive rapid tests always indicate contagiousness, no matter how long it has been since diagnosis.
•How long can I stay contagious? We don’t know for sure. Most people are not contagious after 5 days, which is why the CDC’s guidelines make some sense from the perspective of public health, as mentioned above. A small but important dataset from Japan indicates that 7 to 9 days after symptoms, 19% of infected individuals remained contagious. While none of the asymptomatic cases remained contagious after 5 days, the number of cases was far too small to draw any conclusions. Specifically, if 10% of asymptomatic cases truly are contagious after 5 days, the study would have needed two or three times as many participants to detect that. Meanwhile, I’ve seen positive rapid test results on day 10-12 many times, including among people with no lingering symptoms.
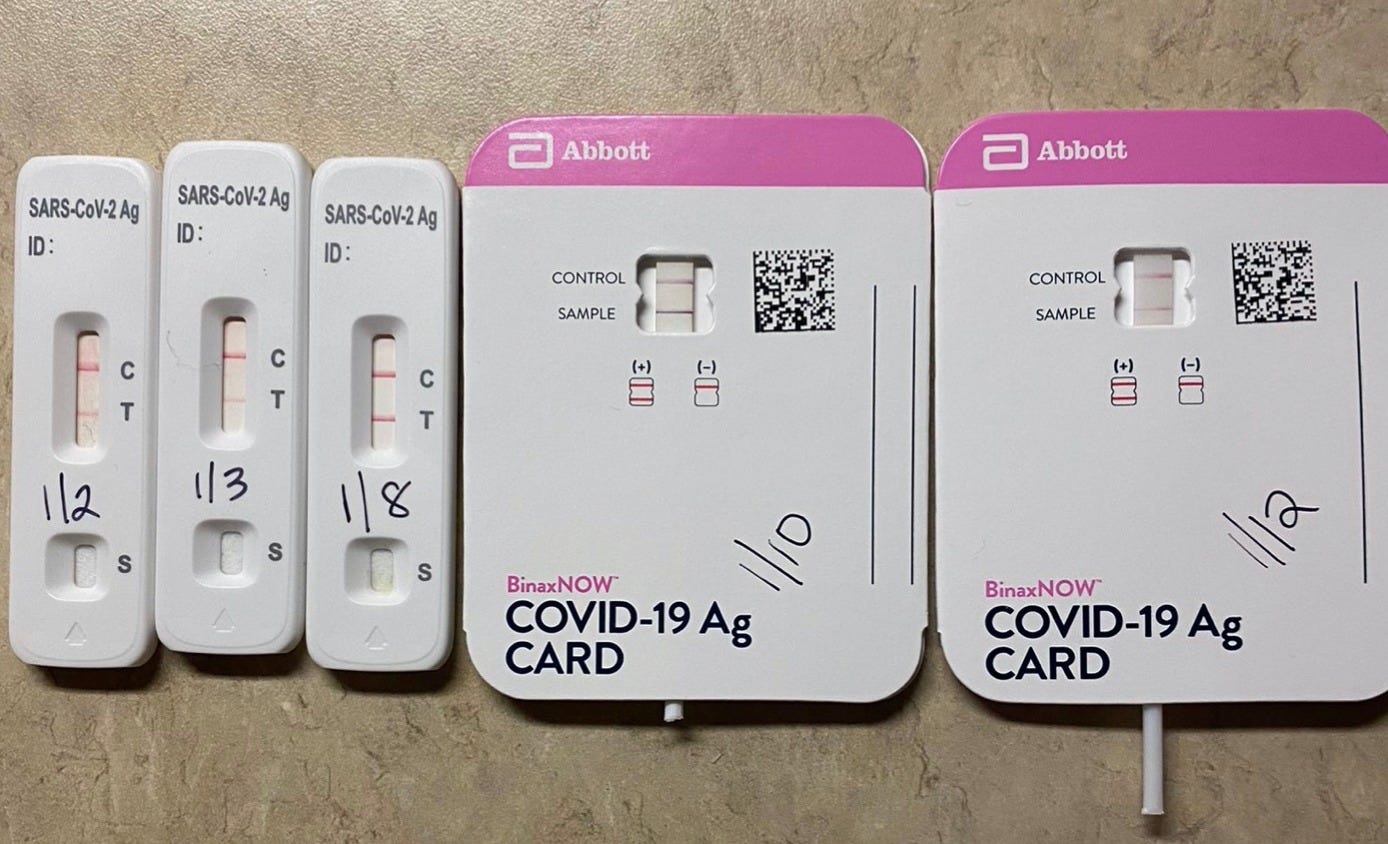
Eleven days of positive rapid antigen tests. This individual's symptoms improved well before finally testing negative.
•••
Interpreting negative at-home rapid antigen tests.
Less straightforward. Prior to Omicron, many of us thought of a negative rapid test as a “day pass.” Now, many of us see the warranty in terms of hours. Overall, interpreting negative results on at-home rapid antigen tests is more complicated, and the stakes are higher if you get it wrong. I’m going to break up the next section into two parts: “I know I’m infected” and “I have no specific reason to think I’m infected.”
Frequently asked questions about negative tests.
•Q: I know I’m infected. How long can I rely on the information from a negative rapid test in the 5 days since I was first diagnosed? A: Not long, if at all. If it has only been a few days since a SARS-CoV-2 diagnosis (or a high-risk exposure without a negative PCR test a few days after), a negative rapid is simply not actionable. I don’t care if you’re boosted or unvaccinated. The virus replicates quickly and you could go from not being contagious to being extremely contagious in a matter of minutes or hours. That said, a negative rapid might reassure someone you were with right before you learned you were infected. Let’s imagine you were tested via PCR yesterday as part of a weekly workplace testing protocol. If you found out at 3pm today that yesterday’s PCR was positive, a negative rapid test now might reassure someone you just spent time with. (What they have to do next depends on their vaccination status, according to the CDC).
•Q: I know I’m infected. Can I rely on negative rapid tests to safely end isolation if it has been longer than 5 days since I was first diagnosed? A: It depends. If you never had symptoms (or they have improved), it is safest if you have had at least two negative rapid tests, at least a day apart, before ending your isolation. Again, the CDC currently says you don’t have to test yourself if you fall into this category though I’d argue that you should if possible. If your symptoms are not getting better, I’d wait longer before testing (let alone interpreting) the results.
•Q: I know I’m infected. I just tested negative on a rapid antigen test. Was that a false negative? A: Not necessarily. Testing negative on a rapid antigen test when you’re infected with coronavirus means you are not likely contagious that instant. In fact, most negative results on rapid antigen tests are not false negatives, even when a person is infected (though some are). It’s impossible to distinguish these two possibilities, however. That’s why if you know you’re infected, you’ll want more than one negative antigen test (a minimum of 5 days after your diagnosis) to start feeling good about not being contagious.
•Q: I have no specific reason to think I’m infected. I just tested negative on a rapid before a dinner party. How long is that information useful to me? A: While any of us could be infected at any time, the odds of being infected and not contagious and then becoming contagious in the following couple of hours after that negative rapid result are pretty low; you’d have to be both unknowingly infected and right on the brink of becoming contagious to be threat to anyone. It can happen, of course, but in my view a negative test directly before an event is fairly safe if you haven’t had any recent high-risk exposures. But during a major outbreak, I’d assume the information to be stale by the next morning.
•Q: I have no specific reason to think I’m infected. If I tested negative on a rapid test a few days in a row, does that rule out a current or very recent infection? A: No. But it certainly lowers the odds. Only a negative PCR test completely rules out a current or very recent (i.e. within the past couple of weeks) infection.

Inside Medicine contributor Benjy Renton's rapid tests during his recent Omicron infection. It looks like his contagiousness peaked on day 7 of his illness, meaning the CDC would have advised him to end his isolation period before he reached maximal contagiousness in the absence of testing. Good thing he stayed home.
•••
Still have questions? Leave them in the comments section. Or just follow Michael Mina on Twitter. Fewer people have been more correct on this topic than Mike. While he now works for a company that markets rapid tests, he didn’t back when he first championed these tests. However, if conflicts of interest bother you, you can be reassured that I don’t have any, since I have never received money from any of these companies.
•••
❓💡🗣️ What are your questions? Comments? Join the conversation below!
Follow me on Twitter, Instagram, and on Facebook and help me share accurate frontline medical information!
📬 Subscribe to Inside Medicine here and get updates from the frontline at least twice per week.