Regular old pneumonia treatment just got better.
An inexpensive steroid made a large difference in a new clinical trial. (If that sounds familiar, you're right).
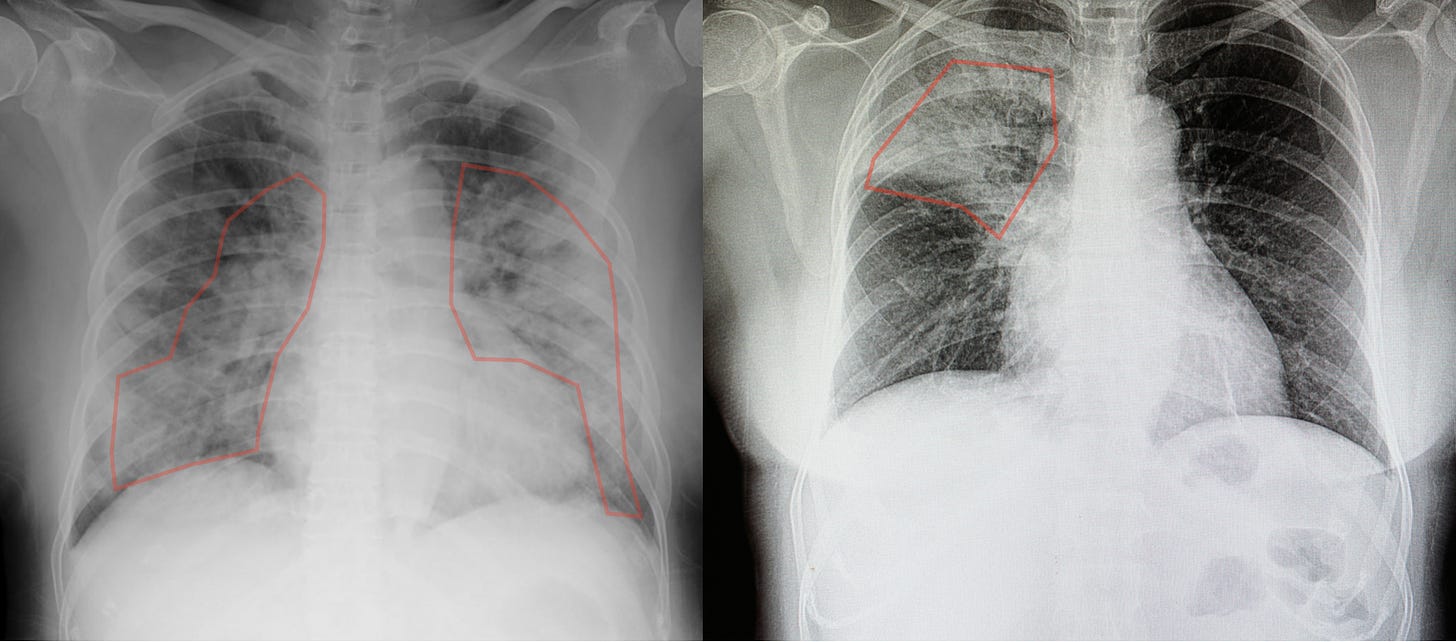
In 2020, Covid-19 pneumonia became so common that “old-fashioned” bacterial pneumonia suddenly seemed rare. They look very different on x-ray. See if you can spot the differences.
Here they are again, but I’ve outlined the bad stuff in red. Notice how Covid-19 shows up in both lungs. That’s classic for Covid.
And again with the bad stuff outlined and shaded in...
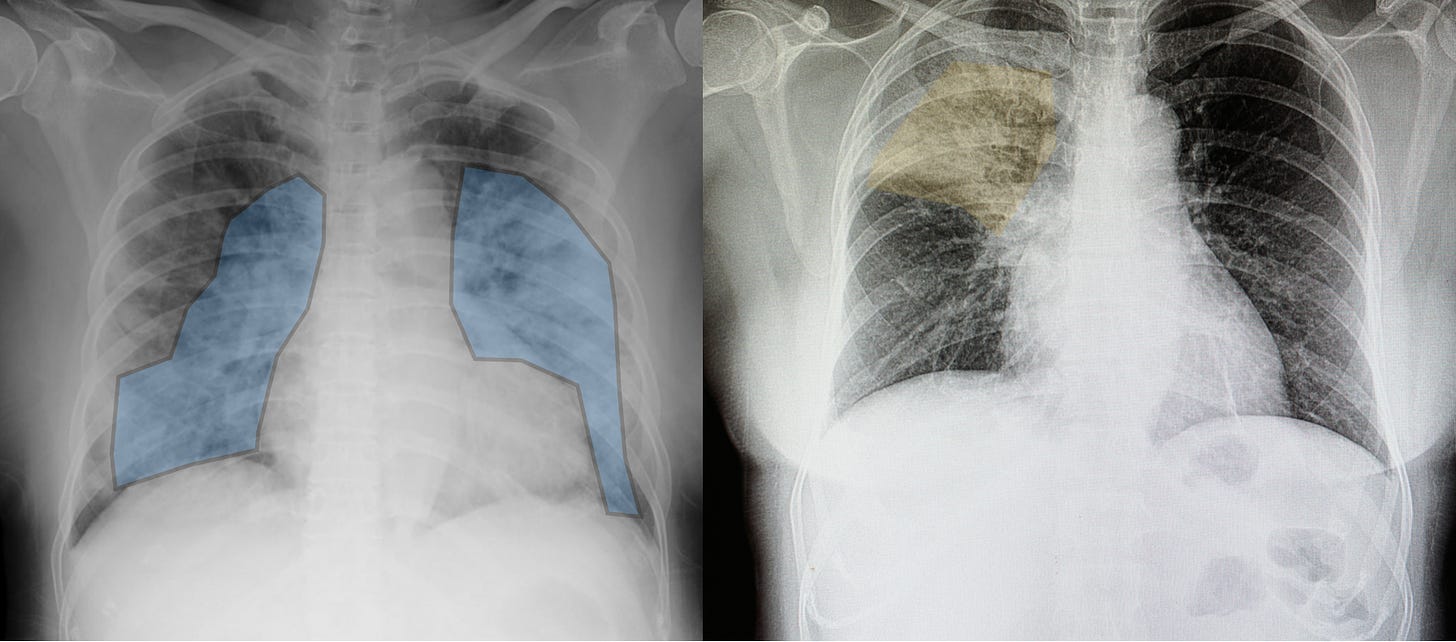
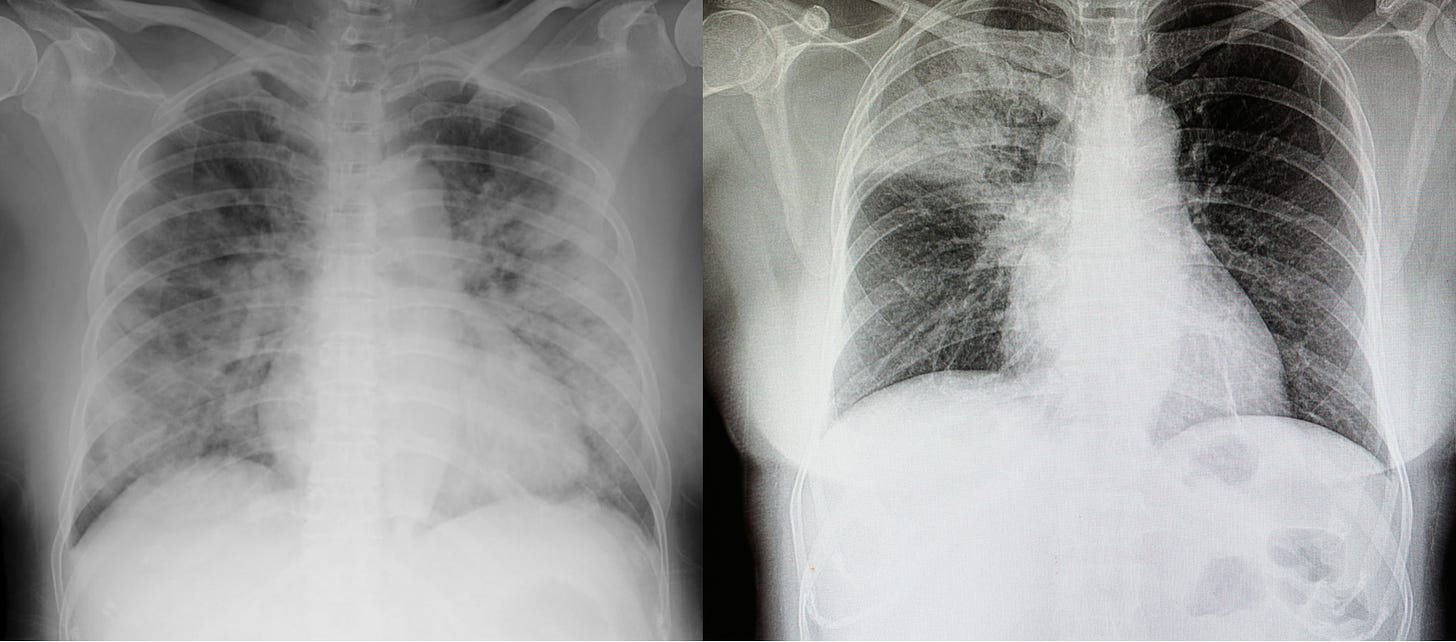
Now got back to the first pair of images and see if you can see it, without the annotations. If you can, congratulations, you’re now a radiologist. (Kind of).
Regular pneumonia once again reigns (on x-ray, anyway).
These days, I’m seeing a lot more of the old kind of pneumonia and less of the typical Covid-19 pneumonia we used to see in 2020 and 2021 before the vaccine and variant eras. People are still dying because of Covid, but as I’ve written before, those deaths don’t “look” like the ones we saw in 2020. So we really are not seeing these x-rays very often.
But we are seeing lots of bacterial pneumonia, just like we always have. Unlike Covid, bacterial pneumonia can usually be treated with antibiotics. But in severe cases, patients need more than that.
For years, there has been a debate in the medical community: Should we give patients with severe bacterial pneumonia steroids?
The new data.
This week, a study from France tipped the scales towards using a steroid called hydrocortisone. This is a stronger intravenous version of the skin cream people use for rashes. (Interestingly, a different steroid called dexamethasone was famously shown to reduce mortality in Covid-19 patients).
In patients with pneumonia severe enough to require the intensive care unit (ICU), 11.9% in the placebo group died, compared to 6.2% in the steroid group. That’s a massive difference for an inexpensive medication (or any). If the research is correct, it means that for every 18 patients with this disease that we give hydrocortisone to, we’ll save one life. I can’t stress how unusual this kind of improvement is in a major study. And the drug is very inexpensive. This is amazing news.
Sex differences.
In the past, the data suggested that women may benefit less from these kinds of steroids in pneumonia. But this trial actually had more women than a well-known earlier study (that had not found steroids to work for this kind of pneumonia). Nevertheless, this latest study found that the steroid worked, both in reducing death and other important outcomes like use of mechanical ventilators and making it out of the ICU. I reached out to the lead author of the study. He didn’t have much of an explanation for the discrepancy between this trial and the previous one, especially in light of the sex differences.
What should you do?
If someone you care about is hospitalized with pneumonia that is severe enough to require the ICU they might benefit from hydrocortisone. It basically comes down to how severe the illness really is, and other factors including whether the steroid is safe for that exact person.
Not every doctor reads the New England Journal of Medicine all the time, and it could take a while for this news to catch on in hospitals. So, you can always just show them this newsletter.
Admittedly, doctors don’t love it when patients’ families breathe down their backs and make “helpful” suggestions like this. My advice is to play it softly. “I read this doctor’s newsletter and he wrote something about some study in the New England Journal about steroids, even for pneumonia that is not Covid. Can I show you?”
Then show them this!
The doctor may agree. Or, they may have very good reasons for why this would not be such a good idea. It’s always more complicated than it may appear. But it never hurts to ask.




My historical perspective on pneumonia: In 1979-80, when I was an intern in NYC, otherwise young, healthy individuals who presented with pneumonia were diagnosed with either pneumococcal pneumonia or mycoplasma pneumonia. Then we began seeing otherwise previously healthy young men present with Pneumocystis carinii Pneumonia which was how AIDS presented before it had been defined.
Interesting choice of steroids. I would have tried prednisone. Also glad to add “radiologist” to my tagline after reading this post, ha! 😜
I’ve been trying ChatGPT with caution for questions at the point of care. Sorry for the long comment but here’s what I got as inspired by this post. After reading this your commenters will also be ICU intensivists, kind of:
Q :
Do steroids help with treating pneumonia for patients in the ICU? Please cite medical references from the New England journal of medicine, Chest journal, and JAMA
A:
There is ongoing debate regarding the use of steroids in the treatment of pneumonia in critically ill patients, including those in the ICU. However, several studies have explored the potential benefits of steroids in this setting.
One study published in the New England Journal of Medicine in 2018, the Steroids in Pneumonia (STRAIN) trial, found that the use of corticosteroids in patients with community-acquired pneumonia who required ICU admission resulted in a significantly lower 90-day mortality rate compared to those who received placebo. The study also found that the steroid group had a shorter time to clinical stability and a lower incidence of treatment failure. (https://www.nejm.org/doi/full/10.1056/NEJMoa1800897)
Another study published in Chest in 2021, which analyzed data from multiple randomized controlled trials, found that corticosteroids reduced mortality and the need for mechanical ventilation in critically ill patients with pneumonia. However, the study also noted that the optimal timing, dose, and duration of corticosteroid treatment in these patients remains unclear. (https://www.sciencedirect.com/science/article/pii/S0012369221001977)
Similarly, a systematic review and meta-analysis published in JAMA in 2020 found that corticosteroid treatment was associated with a lower mortality rate and reduced need for mechanical ventilation in patients with severe pneumonia, including those in the ICU. However, the study also noted that the optimal timing, dose, and duration of corticosteroid treatment in these patients remains uncertain. (https://jamanetwork.com/journals/jama/fullarticle/2766145)
It is important to note that while these studies suggest potential benefits of steroid use in critically ill patients with pneumonia, the decision to use steroids should be made on a case-by-case basis by the treating physician, taking into account factors such as the patient's overall health, the severity of their illness, and potential risks and benefits of steroid therapy.
~
Not bad, right?