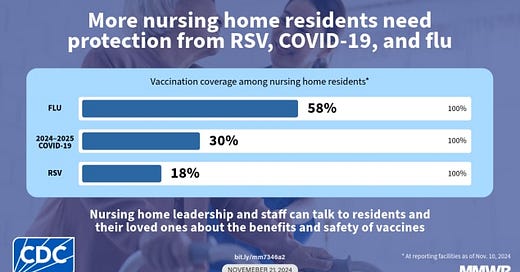
New CDC data show that in nursing homes, rates of flu vaccination are far higher than Covid vaccination so far this fall. As of November 10th, 58% of nursing home residents have received their annual flu shot while just 30% have received a fall Covid vaccine. Meanwhile, RSV vaccine rates are even lower, at 18%.
Most readers of this newsletter take Covid-19 pretty seriously, even while recognizing that the mortality and hospitalization risk of an infection is a fraction of what it was during the pre-vaccine era.
Outside of our echo chamber, though, Covid-19 is often seen as a “thing of the past.” A common talking point we’ve heard about Covid-19 is that it’s “just another flu.” In fact, we’ve heard this from the start of the Covid pandemic. This led my colleague Dr. Carlos Del Rio and me to use data to show otherwise back in 2020; In the first peak of the pandemic, Covid-19 killed somewhere between 9.5-41 times as many people as flu normally does at its peak. Over time, the difference between Covid-19 and seasonal influenza has narrowed, thanks to immunity from vaccines, infections, and the help of therapeutics. Still, even on a per-case basis, Covid-19 remains the more harmful pathogen—not to mention that it causes more infections. That’s a higher batting average and more at-bats, which is not a good combination.
Nursing homes remain a problem.
Early in the pandemic, nursing homes were literal disaster areas. Let’s look at the population aged 65 and older. Around a 26% of all Covid deaths in 2020 occurred in nursing homes, though nursing home residents represent just 0.3% of the US population. An astounding 81,863 people died of Covid while in nursing homes in 2020, which was around 8% of the total nursing home population.
Those figures have fallen by 90%, but the danger is still high; in 2023, over 7,500 nursing home residents died with Covid on their death certificate (as the underlying or contributing cause of death).
Meanwhile, influenza was responsible for a far lower number of deaths in this group. In the worst year in memory (2018), 2,100 people aged 65 and older died of influenza while in a nursing home, or about 0.2% of the nursing home population. But most years, it’s a lot less than that. Now some people think that we undercount influenza deaths and that the system actually fails to detect a majority of flu deaths. Leaving aside the fact that they don’t apply this same “correction” to Covid, even if we somehow miss 5 out of 6 influenza deaths, flu still killed 61% fewer nursing home residents aged 65 and older than Covid did in 2023.
If Covid is more dangerous, why do nursing home vaccinations rates trail flu shots?
Given all of this, you’d think that in nursing homes, Covid-19 would be seen as the bigger threat. You’d also think that Covid-19 vaccination rates would at least be similar to those of flu shot rates, if not higher. But, as we saw above, you’d be wrong.
Why?
I think there are two reasons that Covid-19 vaccine uptake in nursing homes is lower than flu shot uptake.
Reason #1.
First, there are fewer people eligible for a Covid shot this fall. The summer wave of Covid-19 infected a lot of people. According to wastewater analysis by chemical/biological engineer (and clever disease modeler) Jay Weiland, somewhere around 25% of the US population had Covid this summer. Since the CDC recommends waiting at least two months after getting Covid before getting a Covid-19 vaccine, that means a lot of people were not eligible for a Covid shot when the fall rollout began, and many may be waiting until later in the season to get updated. If that’s the case, that’s actually fine, provided that they actually do it as the peak of respiratory virus season begins to approach. In addition, the CDC says that each week in October, around 5,500 nursing home residents got Covid. If we assume that the people who got Covid this summer and fall would have gotten their vaccines at rates similar to those who were eligible and who have received a dose this fall, it looks to me that around 10% of the 28% gap between Covid-19 and flu shot uptake in nursing homes could be accounted for due to this issue. That means that around 40% of nursing home residents would be up-to-date on their Covid shots if they could be, compared to 58% who are currently up-to-date on their flu shot.
Reason #2.
The second reason that fewer people in this group are up-to-date on their Covid shots as compared to flu shots might explain the remaining 18% gap: Perceptions.
For whatever reason, nursing home residents themselves, their families (or health care proxies), and physicians just don’t know the data I shared above. They must think that because people Covid killed 90% fewer nursing homes residents in 2023 than it did in 2020 that the problem is gone. Alternatively, people may not yet be “on board” with the idea that Covid is here to stay and that, like flu, vaccinations should be thought of as a routine part of care for high-risk individuals.
There’s also some politics here. The CDC data show that rates are lower in the South. Covid vaccine rates in nursing homes in HHS Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) are 51% of maximal rates elsewhere (i.e., in more vaccine-friendly parts of the country). This is sad. Vaccines help everyone.
Whatever the reasons—these and others—the vaccine uptake gap between Covid and flu in nursing homes is a major problem. We need to address this and it should be a priority. If we did this, the results would be apparent. Given the risks, it would take a relatively small increase in vaccination rates in nursing home residents to correspond to a saved life. As far as “juice for the squeeze,” you won’t many better opportunities in public health.
How can we fix this problem? Do you have vaccine-hesitant relatives who are also high risk? I’d love to know how you talk about these issues with them. Please join the discussion in the Comments.




I am 62 up to date on my Covid, flu, pneumonia, and RSV vaccines. I am an outpatient dialysis RN and I struggle with some of my patients and vaccines. I give them the facts and tell them I have gotten them all with no issues. Sometimes it helps to tell them I had no issues with the vaccines. I struggle more with family members but most of the time I win.
I have a relative who is in a nursing home in a wealthy town in MA. They’re short staffed. They provide a flu shot, but you have to go to a pharmacy for a covid vaccine. So I keep track of my relatives’ covid vaccines and take her to get them. It’s surprising that a covid vaccine isn’t a standard nursing home option. My experience from visiting a few nursing homes in the state is that they’re often short staffed, and workers call out sick a lot??
I’ve been visiting my relative at this one for 3 years. It seems we as a society… need to pay health care aids and assistants more money to get more workers. Increase the wages for the people who do bedside care, brush teeth, help people get dressed and use bathroom (fall prevention), ambulate with assistance or monitoring etc. ~ encourage eating and drinking water ~ hydration ~ plus a little emotional support and daily conversation …the literal basics for human dignity and basic daily wellness, hygiene, safety. We gotta invest more into these resources and also make long term care actually affordable. Long term care is such a giant economic issue obviously and for families it’s often really difficult in general to navigate and understand. Happy Thanksgiving to all health professionals working on Thursday…and holidays to help others .